What is the difference between heart failure and cardiomyopathy?
Heart failure occurs when the heart does not contract efficiently (systolic failure) or does not relax efficiently (diastolic failure). It does not mean that the heart has stopped working. Heart failure is caused by number of disorders that impair the systolic or diastolic function of the heart muscle including hypertension, coronary artery disease, valvular heart disease and heavy alcohol consumption.
A cardiomyopathy is a condition that causes abnormal structure and function of the heart muscle. There are three types: dilated cardiomyopathy (the most common type), restrictive cardiomyopathy and hypertrophic cardiomyopathy.
What are the symptoms and complications of heart failure?
Symptoms include fatigue, breathlessness and swelling of the legs. The complications of heart failure are fluid retention (with congestion of the lungs, legs and abdomen) and abnormally fast heart rhythms (tachyarrhythmias).
What investigations are useful in diagnosis or management of heart failure management?
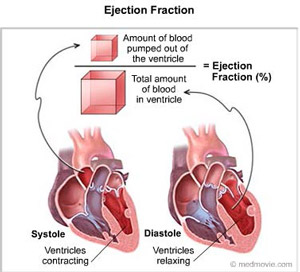
Echocardiography (Echo) is the most useful investigation in patients with heart failure. It provides information about the type (systolic vs diastolic), the underlying cause and the severity of heart failure. Measuring the ejection fraction by Echo is a simple method for quantifying left ventricular systolic function. The Doppler study is particularly useful for assessing left ventricular diastolic function. Electrocardiogram (ECG) and blood tests are routine investigations. Specific investigations such as coronary angiography may then be indicated to confirm the underlying cause or to guide the selection of the appropriate treatment.
How can heart failure be treated?
The underlying cause should be identified and corrected. Heart failure may be treated with the following drugs:
- Diuretics remove the fluid in the lungs and legs. They are often used with aldosterone blockers which improve their efficiency and prevent low potassium levels.
- ACE Inhibitors and ARBs are important drugs because they improve the prognosis in heart failure. They lower the blood pressure and block the compensatory changes that cause congestion and additional strain on the heart.
- An ARNI is a combination of an ARB and a Neprilysin Inhibitor. It can be used in place of an ACE Inhibitor or an ARB.
- Vasodilators reduce the pressure in arteries and veins. They can be used in place of or in addition to ACE Inhibitors and ARBs
- Beta blockers and Ivabridine slow the rapid heart rate that tires the weak heart.
Cardiac rehabilitation improves recovery and response to therapy in heart failure. When heart failure is complicated by certain arrhythmias, a defibrillator or pacemaker device may be implanted to electrically terminate an episode of severe tachycardia or to synchronize the contractility of the weak heart.
What does the Echo look like in heart failure?
Heart Failure
This echo demonstrates a dilated left ventricle with reduced contractility. The ejection fraction is 30%. (The normal ejection fraction is greater than 60%). The patient’s symptoms and ejection fraction improved with medical therapy.